Photodynamic therapy offers promise for cancer treatment
While chemotherapy drugs can be lifesaving, they don’t work for all patients or for all cancers. But a team of UTM researchers is looking at new ways to use special types of light to target cancer cells resistant to current drug therapy—in an approach that might be easier on some patients than traditional chemotherapy.
Photodynamic therapy – the use of precisely targeted light, usually from a laser, that activates or “turns on” a drug to kill cells – has been used mostly to treat skin cancers, since it’s easier to deliver light to the outside of the body. But light doesn’t travel very far through body tissues. So how to safely get the light to cancers that are deeper inside, such as in the pancreas or breast? And how to recognize which cancers will respond to the cell-killing drugs and which will be resistant?
Karishma Kailass, a PhD candidate in the department of chemical and physical sciences, found that using an approach called two-photon light, where two tiny particles of light hit at exactly the same time, achieved this result. It doubled the wavelength, halved the energy and, together with a special cancer-killing molecule that’s activated only by light, successfully destroyed cancer cells that would otherwise have been resistant to conventional chemotherapy.
Kailass says that in creating therapies against cancer, most research focuses on certain proteins that are over-expressed in cancer cells; more of the molecule or drug you’re making will bond to that over-expressed target. “What’s new about what we’ve done,” she explains, “is we’ve taken an approach that targets something that is under-expressed in cancer.” The drug-resistant pancreatic and breast cancer samples the team examined showed low levels of a protein called carboxylesterase 2. Since that’s the very protein targeted by the most common chemotherapy drugs, cancers with low levels would be resistant.
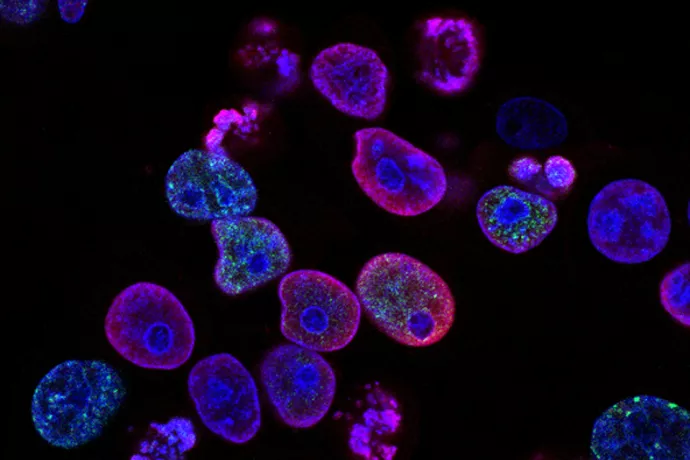
The levels of this protein vary from individual to individual, but using the two-photon light causes the molecule to show different colours of fluorescence depending on the level: when there are high levels of the protein present, it fluoresces red; with low levels, it fluoresces yellow. “This way you can tell whether the patient will be responsive or resistant to chemotherapy,” Kailass says. “And then if they are resistant, you can use the molecule itself to actually treat them.”
The therapy can be extremely precise. For cells that are red – showing high levels of the protein – conventional chemotherapy would work but the molecule wouldn’t, because the protein would break it down. For cells that are yellow – and resistant to regular chemotherapy – the molecule would retain its form, and the two-photon light would activate it to kill the cancerous cells. This approach is expected to be easier on patients, take less time and be done on an outpatient basis, using an IV to administer the photosensitizer molecule so that it settles into the tumour site, and fibre-optic technology for delivery of the light. The research has so far been done only in the lab, but Kailass says the next steps are animal studies and then, it’s hoped, clinical trials in humans.
Kailass’s findings came about by happy accident, when she used the wrong light in the middle of an experiment looking at how photosensitive the molecule was. “I took the purple light to shine on the yellow when I was supposed to take the green light to shine on the red,” she says, laughing. She watched in surprise as the molecule produced an increase in cancer-killing properties. “Hmm, haven’t seen that before!” she thought. Realizing her mistake, she went on to reproduce the study, whose findings were published in June in the Journal of Medicinal Chemistry.
Kailass works in the laboratory of chemistry professor Andrew Beharry, who calls her “exceptionally talented.” Looking toward the future, he adds, “We envision our molecule to help clinicians with drug-decision making, as well as providing them with a novel therapeutic that kills cancers differently than conventional chemotherapeutic drugs.”



